- HPI: middle aged woman presenting with pulmonary edeam, chest pain 2 wks earlier
- Cath: 100% thrombotic mid-LAD occlusion was found; peak cTnT 8.7
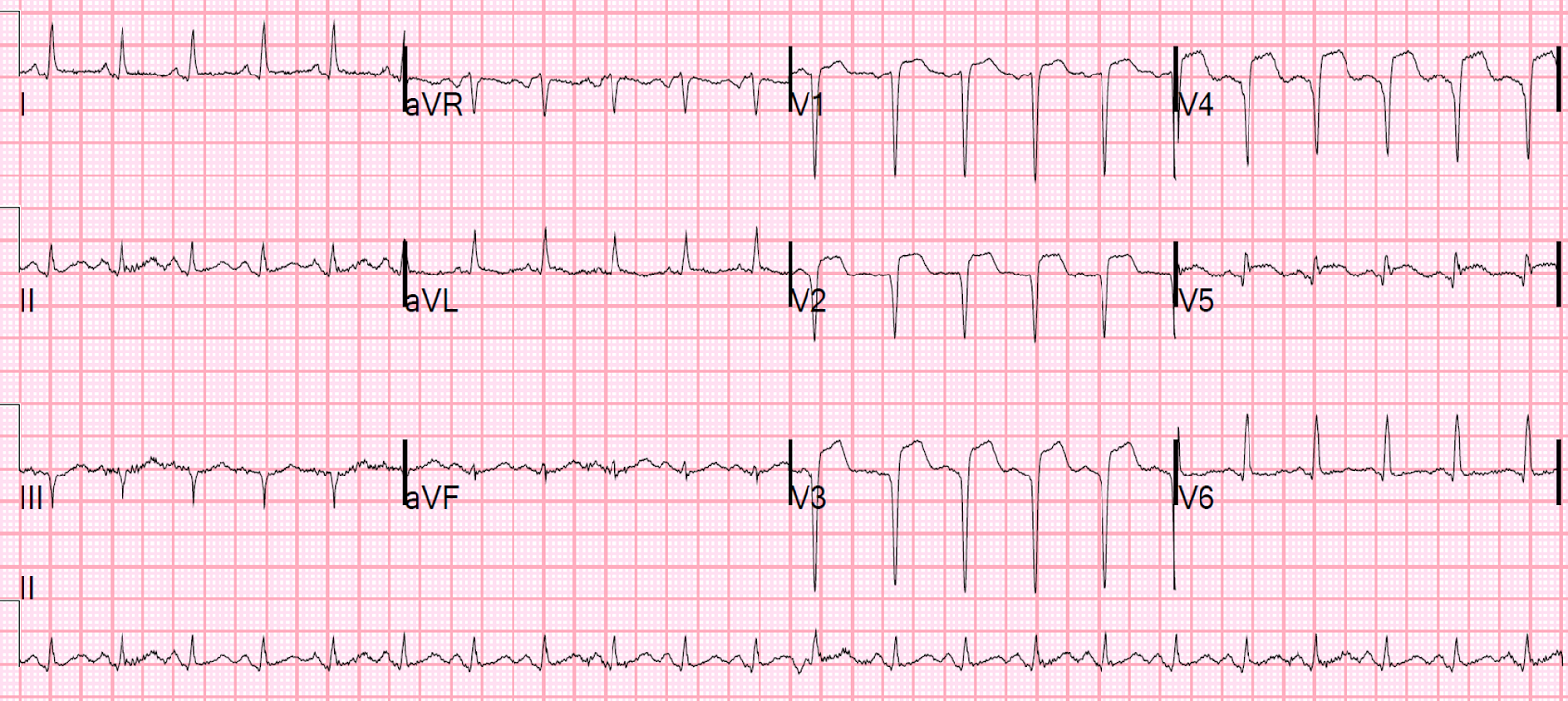
- Key ECG: This likely represents subacute STEMI. Dr. Smith’s rule for differentiating acute STEMI from LV aneurysm really only reliably distinguishes between: 1. acute STEMI on the one hand 2. subacute STEMI or LV aneurysm on the other. First, there must be ST Elevation. Second, the ECG differential diagnosis much be LV aneurysm vs. acute STEMI. When should LV aneurysm be on the ECG differential diagnosis? Primarily when there are well-formed Q-waves, with at least one QS-wave, in V1-V4. A QS-wave is defined by absence of any R-wave or r-wave of at least 1 mm. (If there is an R-wave or r-wave, we call the whole wave a QR-wave, Qr-wave, or qR-wave, depending on the relative size of the Q-wave vs. R-wave.) The rule: If there is one lead of V1-V4 in which the T/QRS ratio is greater than 0.36, then acute STEMI is the likely diagnosis, though subacute STEMI is also possible. Since both require the cath lab, if the ratio is greater than 0.36, and the clinical situation is right (i.e., unexplained chest discomfort), then cath lab activation is should be considered. If the formula were used here, then lead V4 would have a T/QRS ratio of 5/11.5 = 0.43. Only one lead is needed, so the criterion is met for acute STEMI. Really, however, LV aneurysm was never on Dr. Smith’s differential diagnosis when he glanced at this ECG. Why? It is true that there are QS-waves in all of V1-V4, which might lead you to believe it is LV aneurysm. However, this ECG has up to 4 mm of ST elevation (in V4, 4 mm STE is relative to an 11.5 mm S-wave), and Dr. Smith has never seen an LV aneurysm case with this much ST elevation.
- Link to full case @ Dr. Smith’s ECG Blog: 2017-04-21